|
Endoscopic assisted posterior decompression for spinal neoplasms
Ralph J. Mobbs1 BSC(MED), MB,BS, Peter Nakaji1 MD, Bartek J. Szkandera2, Charles Teo1 MD, FRACS
1 Centre for Minimally Invasive Neurosurgery, The Prince of Wales Private Hospital and 2 University of New South Wales, Randwick, Sydney
Summary The authors describe a technique for anterior thoracic decompression via a posterolateral approach for spinal metastatic disease
followed by anterior and posterior column stabilization. We discuss the benefits of decompression via a posterolateral approach including
minimization of cord retraction, avoidance of thoracotomy, early mobilization and shorter hospital stay. Technical details are reviewed and
difficulties of the approach discussed. & 2002 Published by Elsevier Science Ltd.
Keywords: endoscopy, decompression, posterolateral approach, neoplasia
INTRODUCTION
Endoscopic assisted spinal surgery is becoming widely accepted as an adjunct to established open techniques in spinal surgery. The aim of our report is to describe an alternative approach for the treatment of anterior thecal compression from thoracic metastatic disease.
Skeletal metastasis commonly develop in carcinoma patients with the spinal column being the most common site of secondary disease.1 As patient longevity improves, spinal surgeons will be presented with more patients suffering from symptomatic cord compression. Standard anterior vertebral
body resection via thoracotomy results in prolonged ICU and hospital stay. In the future we will be forced to adapt to new techniques to reduce morbidity and reduce hospital stay.
TECHNICAL CASE REPORT
A 62 year old male presented with back pain of several weeks duration. Initial CT of the lumbosacral spine was normal.Examination of the lower limbs revealed mild hyperreflexia, otherwise a normal examination. An MRI scan of the spine was performed which revealed a lesion in the posterior aspect of the T11 vertebral body with extension into the right pedicle (see Figs 1 and 2). Thorough investigation revealed a large
lesion in the left kidney and a provisional diagnosis of renal cell metastasis to the T11 vertebra was considered the most likely scenario.
Due to the moderate dural compression and hyperreflexia, a decision to remove the vertebral metastasis was made. The vertebral lesion was embolized 48 h prior to surgery to reduce problematic intraoperative bleeding. Under general anaesthesia in the prone position on a Wilson frame, a midline incision was made to reveal T9±L1 spinous process, lamina and transverse processes. A perpendicular incision on the right was made to
reveal the paraspinal musculature to its lateral border. Upon elevation of the paraspinal muscles, the T11 rib was visualized. The medial aspect of the T11 rib was excised to the T11 transverse process. The rib removed was kept for bone grafting at the completion of the procedure.
A costotransversectomy was performed and tumour encountered at the posterior aspect of the pedicle. Tumour removal was carried out until the pedicle was removed and a clear corridor available for introduction of the endoscope via a lateral approach (Fig. 3). Tumour removal under endoscope assisted control was accomplished with the aid of curettes and bipolar diathermy until a compete macroscopic clearance achieved. A Pyramesh titanium cage (Soframor-Danek) was packed with bone graft and impacted into the defect between T10±T12 for anterior column stabilization (Fig. 4). Methylmethacrylate was also inserted into the dead space arround the cage. Fixed angle pedicle screws (HorizonTM Soframor-Danek) were inserted into T10 and T12 with rods
and cross link for posterior column stabilization. The patient had an endoscopic nephrectomy 10 days following his spine surgery without complication. He was discharged 3 days postnephrectomy. At follow up 2 months from surgery the patient appears well with no back pain or hyperreflexia and has returned to independent living.

Fig. 1 Tumour in the posterior aspect of T11 vertebral body with dural compression.

Fig. 2 Tumour occupying the lateral aspect of the vertebral body and pedicle.
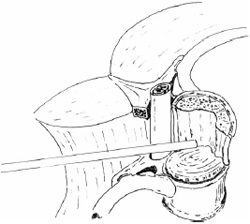
Fig. 3 Approach angle of endoscope to view tumour without cord manipulation.
DISCUSSION
Microsurgical endoscopy for thoracic metastasis is not a
new idea.2,3 Rosenthal et al. (1996) attempted anterior decom-
pression via a multiport thoracoscopy technique and recon-
struction using methylmethacrlyate and Z-plate in 4 patients.2
McLain (1998) described a technique similar to this report
using transpedicular endoscopy for thoracic metastatic disease
in 5 patients.3 Our technical report adds to this early body literature to broaden the techniques available for decompression of thoracic metastatic disease.
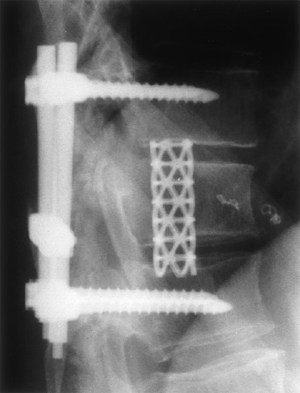
Fig. 4 Postop lateral X-ray: anterior and posterior column stabilization.
Advantages that we encounted include minimal retrac-
tion/manipulation of the cord, precise localization of bleeding
points aiding haemostasis and heightened appreciation of the
bony anatomy to help with anterior reconstruction. Dis-
advantages encountered include the need for a lateral corridor
for introduction of the endoscope and thus a more extensive
initial lateral dissection and additional time taken for set up of
the endoscope. A potential disadvantage that has been dis-
cussed by previous authors includes the `spray' from high speed
drills when using the endoscope.4 We minimized this problem
by predominantly using curettes for the bone work during
tumour removal. As a surgeon uses the endoscope more often,
the time taken for set up and the learning curve in tolerating a
2D environment will become less challenging.5
The authors adopted an aggressive approach to tumour
removal in this patient as the evidence for longer survival with
renal cell metastasis is related to the degree of tumour resec-
tion.6 The 2 year survival for patients with spinal metastasis
from renal cell carcinoma is 37% in the group with complete
tumour resection versus 0% in the group treated with radio-
therapy alone.7
Endoscopic assisted decompression can reduce morbidity,
hospital stay, and treatment costs while matching the efficacy
of traditional combined procedures.5 Endoscopy provides a
readily available and easily applied tool that dramatically
improves the surgeon's vision, providing light, magnification,
and a direct view of remote structures.
REFERENCES
- Galasko CSB. The anatomy and pathways of skeletal metastasis.
In: Weiss L, Gilbert HA (eds). Bone metastasis. Boston: GK Hall
Medical Publishers, 1981; 49±63.
- McLain RF. Endoscopically assisted decompression for metastatic
thoracic neoplasms. Spine 1998 May 15; 23(10): 1130±1135.
- Rosenthal D, Marquardt G, Lorenz R, Nichtweiss M. Anterior
decompression and stabilization using a microsurgical endoscopic technique
for metastatic tumors of the thoracic spine. J Neurosurg 1996 Apr; 84(4):
565±572.
- Mobbs RJ Teo C. Endoscopic assisted posterior fossa decompression.
J Clin Neurosci 2001 Jul; 8(4): 343±344.
- Teo C. Endoscopic-assisted tumor and neurovascular procedures.
Clin Neurosurg 2000; 46: 515±525.
- Saitoh H, Hida M, Nakamura K, Shimbo T, Shiramizu T, Satoh T.
Metastatic processes and a potential indication of treatment for metastatic
lesions of renal adenocarcinoma. J Urol 1982 Nov; 128(5): 916±918.
- Sundaresan N, Scher H, DiGiacinto GV, Yagoda A, Whitmore W, Choi IS.
Surgical treatment of spinal cord compression in kidney cancer. J Clin
Oncol 1986 Dec; 4(12): 1851±1856.
 Endoscopic Assisted Posterior Decompression Endoscopic Assisted Posterior Decompression
You will need the Adobe Reader to view and print the above documents. 
|
