|
Mesh electrode for peripheral nerve stimulation
Ralph J. Mobbs1
BSC(MED) MB BS, Peter Blum2
MB BS (SYD) FRCS(GLAS) FRACS, Reno Rossato3
MB BS FRACS
1Peripheral Nerve Research Foundation, Randwick, Sydney, Australia, 2Department of Neurosurgery, Institute of Neurological Sciences, The Prince of Wales Hospital, Sydney, Australia, 3Calvary Hospital, Cairns, Queensland, Australia
Summary The implanted peripheral nerve stimulator has a role for pain relief in well-selected patients with pain in a peripheral nerve
distribution. We describe an electrode to help simplify the surgical implantation of a peripheral nerve stimulator and also to reduce the possibility of electrode migration following implantation. Design details of the electrode are discussed, as are notes on surgical technique.
© 2003 Elsevier Science Ltd. All rights reserved.
Keywords: peripheral nerve, electrode, stimulator
INTRODUCTION
Following the gate control theory that stimulation of large diameter afferent fibers can interrupt the transmission of nocceptive input,1 electrical stimulation of peripheral nerves using implanted and transcutaneous electrodes has been used over the past 40 years.2 Wall and Sweet3 first described an implanted peripheral nerve electrode in 1967. The results were mixed with an initial good response followed by a decline. Since then, there has been many reported series in the literature documenting the results of these implantable devices.4–6 Initially, circumferential electrodes for treating mononeuropathies were used. These gave way to paddle type electrodes (Resume electrodeTM, Medtronic, Minneapolis, USA). Difficulty securing these electrodes resulted in electrode migration and failure of the device, both short and long
term. The senior author (P.B.) has a series of over 40 implanted peripheral nerve stimulators, larger than any published series. Design modifications discussed here were made with an attempt to improve ease of intraoperative application of the electrode and also to minimize the complication of lead migration.
TECHNICAL NOTE
The modified Resume electrode consists of two design modifications. The first is the unilateral mesh (Fig. 1). The mesh was added to the standard design to help secure the electrode to the nerve requiring stimulation. The mesh is wrapped around the nerve and the addition of a suture(s) to secure the device to adjacent fascia is possible. The second modification is the offset lead. The lead is normally attached to the electrode in the midline on a standard Resume electrode, however, the lead offset helps with “seating” the electrode in the wound as the surgeon can view the lead take-off with the electrode in position. Implantation of a nerve stimulator is a two-stage procedure.
Following confirmation of the nerve to be stimulated, the initial operation involves exposure of a proximal section of the affected nerve under general anesthesia. Positioning of the nerve stimulator should not be over or adjacent to a joint as this may result in failure of the device due to electrode migration with joint movement. Intraoperative direct stimulation of the nerve may be used to assist anatomical confirmation of the nerve that has been exposed. The segment of nerve exposed should be only enough to apply the stimulator in order to reduce incision size and scar formation. A thin layer of fascia is left over the nerve prior to electrode application. The modified Resume ™ electrode is positioned on the deep aspect of the nerve (see Fig. 2). The patient is less likely to notice the device if the firm plate of the electrode is deep to the nerve rather than superficial. The mesh is wrapped around the nerve and secured with a non-absorbable suture in an interrupted fashion; such as 4/0 Nylon (see Fig. 3). The lead offset (Fig. 1) aids in positioning the electrode in the deeper surgical planes. A trial lead is connected to the Resume electrode and exits the skin. The trial generator is attached on day 1 following surgery. A
Medtronic representative instructs the patient on the use of the generator so that the patient can find a setting that best suits their
pain profile.
Following a trial period of 3–7 days of nerve stimulation, a decision
is made in consultation with the patient if the device is to be
permanently implanted. As a general rule, for stage 2 to proceed, the
patient must have attained at least a 50% reduction in pain scores
and have no significant morbidity such as adjacent muscle twitching
or lead discomfort. Poor electrode placement can lead to annoying
stimulation of adjacent structures and require re-positioning. We do
not believe that a trial period of 1–2 days is adequate, as the patient
may not yet have returned to full mobility or their usual daily routine.
The second stage is performed under general anesthetic. Position
of the battery/generator in the chest wall is decided
preoperatively in consultation with the patient. Tunneling of a lead
from the electrode to the battery/generator is required and performed
with a provided tunneling device. Be sure to leave some
“slack” in the tunneled lead as the patient may complain of skin
tenting and discomfort if the lead is tight. This is most obvious with
the upper limb in abduction. During stage 2, we move the arm into a
flexed, then an abducted position to assure that the lead does not
limit upper limb movement.

Fig. 1 An early design of the modified Medtronic ResumeTM electrode with
unilateral mesh and offset lead.
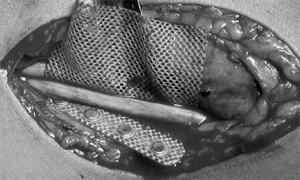
Fig. 2 Modified ResumeTM electrode positioned deep to an ulnar nerve prior
to wrapping and anchoring by suture .
 g g
Fig. 3 Mesh around the nerve to secure the electrode and prevent
migration.
DISCUSSION
Although there is still debate as to the long-term effectiveness of
implantable peripheral nerve stimulators, the authors believe that
initial secure and accurate implantation of the electrode is paramount
to success. In our own series of 41 long-term implanted
stimulators, 8 (19.5%) have required revision due to lead migration
or morbidity due to stimulation of adjacent structures. The
addition of the modified electrode in the latter part of the study
period reduced the frequency of electrode repositioning. The
offset lead facilitates implantation, especially if the electrode is
positioned deep to the nerve. The mesh fixation reduces the risk of
electrode migration due to limb or lead movement. In conclusion,
the advantages of the modified electrode are easier surgical implantation
and reduced in lead migration.
ACKNOWLEDGEMENTS
We would like to thank Mr. Phil Bragg of Medtronic Australia for
providing details of lead development. No grants of any kind were
used in the preparation of this article.
REFERENCES
- Melzack R, Wall PD. Pain mechanisms: a new theory. Science 1965; 150: 971.
- Novak CB, Mackinnon SE. Outcome following implantation of a peripheral nerve
stimulator in patients with chronic nerve pain. Plast Reconstr Surg 2000; 105(6):
1967–1972.
- Wall PD, Sweet WH. Temporary abolition of pain in man. Science 1967; 155:
108–109.
- Picaza JA, Cannon BW, Hunter SE, Boyd AS, Guma J, Maurer D. Pain
suppression by peripheral nerve stimulation. Part II. Observations with implanted
devices. Surg Neurol 1975; 4(1): 115–126.
- Hassenbusch SJ, Stanton-Hicks M, Schoppa D, Walsh JG, Covington EC. Longterm
results of peripheral nerve stimulation for reflex sympathetic dystrophy. J
Neurosurg 1996; 84(3): 415–423.
- Campbell JN, Long DM. Peripheral nerve stimulation in the treatment of
intractable pain. J Neurosurg 1976; 45(6): 692–699.
 Mesh Electrode for Peripheral Nerve Stimulation Mesh Electrode for Peripheral Nerve Stimulation
You will need the Adobe Reader to view and print the above documents. 
|
