|
Technical Note: The 80/20 Technique for Posterior Lumbar Interbody
Fusion – A Combination of Open Decompression and Percutaneous
Pedicle Screw Fixation
Ralph J Mobbs1,2,3, Praveenan Sivabalan2,3*, Jane Li2,3 and Peter Wilson1,2
1Department of Neurosurgery, Prince of Wales Private Hospital, Australia
2Neuro Spine Clinic, Randwick, New South Wales, Australia
3University of New South Wales, Kensington, New South Wales, Australia
Abstract
Objective: To illustrate a hybrid technique that involves a combination of open decompression and Posterior
Lumbar Interbody Fusion (PLIF) and percutaneously placed pedicle screws. This technique allows for PLIF via a midline
incision and approach, and decompression without compromise in operative time and visualisation. Furthermore, this
approach is proposed to reduce post-operative wound pain by: smaller midline incision, significantly reduced muscle
trauma by not dissecting the paraspinal muscles off the facet joint complex, avoidance of a posterolateral fusion to
facilitate limited lateral muscle dissection off the transverse processes.
Summary of background data: PLIF fusion rates are comparable to posterolateral fusion rates, as well as
providing greater sagittal and coronal balance. There is positive evidence that degenerative spondylolisthesis with
canal and/or foraminal stenosis requires stabilisation when decompressed via laminectomy.
Methods: Patients with Grade I-II spondylolisthesis at L4/5 with moderate - severe canal/foraminal stenosis
undergo a midline PLIF at L4/5, with closure of the midline incision. Percutaneous pedicle screws are inserted,
therefore minimising local muscle trauma, with reduction of the spondylolisthesis performed using the pedicle screw
construct. Rods are inserted percutaneously to link the L4 and L5 pedicle screws. Image intensification is used to
confirmed satisfactory screw placement and reduction of the spondylolisthesis.
Conclusion: Percutaneous lumbar pedicle screws can be combined with a standard midline PLIF to reduce postoperative
wound pain while allowing for satisfactory screw placement.
Keywords: Percutaneous lumbar pedicle screws; Posterior lumbar
interbody fusion; Spondylolisthesis; 80/20 technique; 50/50 technique
Introduction
Degenerative lumbar spondylolisthesis provides a challenging
clinical entity. When associated with lumbar canal and/or foraminal
stenosis the patient can present with claudicant and/or radicular
symptoms respectively. Positive outcomes can be seen with operative
intervention when compared to conservative management. The
spondylolisthesis arm of the SPORT trial concluded that in a
nonrandomised as-treated environment (with control of potentially
confounding baseline factors), outcomes were significantly better in
regards to pain and function after 2 years for patients with degenerative
spondylolisthesis and spinal stenosis than those treated non-operatively
(SPORT Trial) [1]. Its correlation with mechanical low back pain is less
clear and will not be discussed here.
One of the treatment methods proposed for degenerative
spondylolisthesis with claudicant and/or radicular symptoms is lumbar
laminectomy with instrumented fusion. This can take the form of a
posterior approach (pedicle screw fixation ± posterolateral graft ±
posterior or transforaminal lumbar interbody fusion: PLIF/TLIF), as
well as an anterior approach (anterior lumbar interbody fusion: ALIF),
or a combination of the above. PLIF has been shown to be equivocal
to TLIF in regards to good outcomes post-operatively [2]. PLIF has
been shown in one prospective study to have a higher fusion rate than
posterolateral fusion alone, but at the cost of a higher complication
rate related to hardware biomechanics [3]. Kim et al. [4], found that
in directly comparing PLIF, posterolateral fusion and PLIF with
posterolateral fusion, that there was no difference in regards to clinical
results and union rates between the three; however, they noted that
PLIF alone allowed for less donor site pain, shorter operating time and
less blood loss (it has been noted that these benefits are, at least in part,
attributable to not taking any iliac crest bone graft for the PLIF group)
[4]. In a review of PLIF versus posterolateral fusion for management of
isthmic spondylolisthesis, a higher fusion rate of 93% for PLIF versus
68% for posterolateral fusion was found, but only with a statistically
significant improvement of outcome for high grade slipping managed
with PLIF; there was no difference in outcomes for low grade slip [5].
An earlier review noted improved statistical parameters for PLIF over
posterolateral fusion in isthmic spondylolisthesis, but without any
clinical outcome variation [6].
Disadvantages of an open posterior approach include the morbidity
of increased muscle dissection, increased post-operative wound pain
(both short and long term), slower mobilisation post-operatively (and
subsequent longer hospital stay), as well as increased intra-operative
blood loss. An alternative method to the “traditional” open approach is
to provide a minimally invasive method by use of percutaneous pedicle
screws in combination with a minimally invasive bilateral laminotomy
and PLIF. However, this method is compromised by longer operating
times and higher complication rates [7].
*Corresponding author: Praveenan Sivabalan, Suite 3, Level 7, Prince of Wales
Private Hospital, Randwick NSW 2031, Australia, Tel: +61-4-0196-5057; Fax: +61-2-
9650-4943; E-mail: praveenan_sivabalan@hotmail.com
Received February 02, 2012; Accepted May 28, 2012; Published June 10, 2012
Citation: Mobbs RJ, Sivabalan P, Li J, Wilson P (2012) Technical Note: The
80/20 Technique for Posterior Lumbar Interbody Fusion – A Combination of
Open Decompression and Percutaneous Pedicle Screw Fixation. J Spine 1:119.
doi:10.4172/2165-7939.1000119
Copyright: © 2012 Mobbs RJ, et al. This is an open-access article distributed under
the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution, and reproduction in any medium, provided the original author and
source are credited.
An alternative method that is presented here involves a combination
of the open and minimally invasive approaches, with the aim of
maximising the benefits and avoiding the disadvantages of both the
open and minimally invasive approaches. An open laminectomy and
PLIF is performed at the pathological disc level to minimise operative
time and to provide adequate exposure. This allows minimisation of
intra-operative adverse events as well as provide a contingency in the
event of adverse events should they occur (e.g. incidental durotomy).
A PLIF alone is used and a posterolateral graft is excluded to minimise
muscle dissection and retraction laterally, without compromising rates
of fusion. Finally, percutaneous pedicle screws are placed in all pedicles
to minimise muscle dissection off the facet joints to minimise postoperative
wound pain (Figure 1).
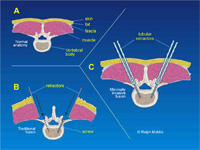
Figure 1: Rationale for MIS pedicle screw fixation: Minimization of muscle
trauma with percutaneous pedicle screw insertion technique.
Technical Note
The “80/20 Technique” (Figure 2) name was coined by the senior
author (RJM) to describe the relative importance of each step in the
procedure. The initial “80%” is the primary goal of the technique:
decompression of the neurological elements, preparation of the
vertebral endplates and insertion of an interbody cage on either
side of the thecal sac (Figure 3). The final “20%” is the percutaneous
insertion of the pedicle screws and reduction of the spondylolisthesis.
The senior author has also previously described the “50/50 Technique”
(Figure 4). In this case, the caudal pedicle screws are inserted via an
open approach. This technique may be required if the caudal pedicle
anatomy is difficult to determine using Anterior-Posterior X-ray and
the surgeon is not comfortable with inserting percutaneous pedicle
screws at that level.
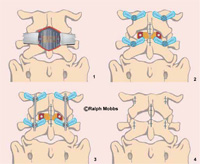
Figure 2: Workflow with 80/20 technique: 1. Midline incision and Posterior
Lumbar Interbody Fusion performed. 2. Closure of the midline incision. 3.
Percutaneous screw insertion via x4 incisions with reduction using the pedicle
screw construct. 4. Closure of the percutaneous incisions.
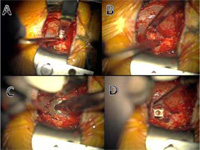
Figure 3: Midline PLIF Technique via Mini-open approach: A. Midline incision,
decompression and preparation of interbody (disc) space. B. Endplate
preparation. C. Insertion of rotatable cage packed with graft. D. Interbody
cage in position.
The 80/20 Technique is as follows:
Step 1: Under general anaesthesia, the patient is positioned prone
on the Jackson table or similar operating table. It is essential to allow
a radiolucent operative table at the level of the surgery to facilitate
anteroposterior (AP) image intensifier x-rays.
Step 2: A midline incision is performed directly over the L4/5
disc space using X-ray to confirm the level of the spondylolisthesis.
Lateral retraction is not necessary and therefore a short incision only
is required. Most incisions are between 3.5-5 cm. A retractor system of
the surgeons’ choice is used and a laminectomy at L4/5 is performed.
A bilateral medial facetectomy at L4/5 with rhizolysis of both L5 nerve
roots is undertaken. The disc at L4/5 is then removed and the endplates
prepared (Figure 3). The bone from the L4 spinous process, laminae
and L4/5 facets was cleaned of residual ligament/soft tissue and milled
using a bone mill. It was then combined with osteobiologic material
before being packed into two PLIF cages and inserted into the L4/5
disc space. After haemomstasis, the midline wound was closed in layers
(Figure 2).
Step 3: The X-ray/II machine is moved into position to target the
L4 and L5 pedicles. A Jamshidi needle is introduced via a stab incision
along the lateral aspect of the pedicle on the AP view. The Jamshidi is
introduced into the pedicle to a depth of 20-25mm making sure not to
breach the medial border of the pedicle wall on the AP view. Lateral
X-ray is performed to confirm the position of the Jamshidi into the
vertebral body. After confirmation of the pedicles being penetrated by
the needle, the trochar is removed and Kirschner (K)-wires introduced
down the barrel of the Jamshidi needle. Their position is then confirmed
prior to advancement of the K-wire through the pedicle under lateral fluoroscopy. Once a satisfactory penetration of the pedicle with the
K-wire was completed, the Jamshidi needle is removed whilst taking
care to keep the K-wire in the same position. Appropriate skin incisions
then need to be made. A pedicle tap is introduced down the K-wire,
through the pedicle into the trabecular bone of the vertebral body and
is confirmed with the image intensifier. The tap is then removed and
appropriate pedicle screws (measurements based on pre-operative CT
scans) were sited. Confirmation of pedicle screw placement is achieved
with the image intensifier. Reduction of the spondylolisthesis is then
performed using the instrumentation of the surgeon’s choice (Figure
5). At the completion of the case, the 4 stab incisions are closed (Figure
2) with a single suture for the deep fascial and a single suture for the
skin incision.
Step 4: Following reversal of anaesthesia, the patient is extubated
post-operatively and transferred to the ward. Mobilisation can be
attempted from day 1 post-op. Post-operative CT of the lumbar spine
allows confirmation of reduction of the spondylolisthesis, as well as satisfactory positioning of the interbody devices, bone graft and all four pedicle screws. Follow up is routinely performed at 6 weeks and
3 months with flexion/extension x-rays views to confirm a solid fusion
and reduction of the spondylolisthesis at L4/5.
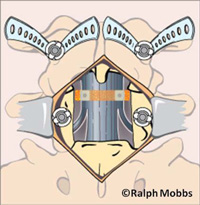
Figure 4: Workflow with 50/50 technique: Midline incision and Posterior
Lumbar Interbody Fusion performed and insertion of pedicle screw into the
caudal pedicle. Insertion of percutaneous screw into the cranial pedicle,
therefore avoiding damage of the cranial/mobile facet joint.
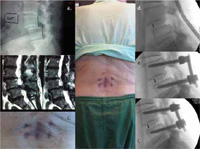
Figure 5: Pre and Post Operative Case example: A) L4/5 Spondylolisethesis.
B) Severe canal stenosis. C) Final appearance of incisions at 4 weeks
postop. D) Initial posterior lumbar interbody fusion performed. E) Insertion
of percutaneous screws. F) Reduction manouver and correction of
spondylolisethesis.
Clinical Results
A clinical study was conducted from 2007 – 2011 to compare
the prospective results of open versus minimally invasive fusion
(80/20 technique) for degenerative lumbar spine pathologies. Eightytwo
patients were studied (41 MIS spinal fusion, 41 open surgical
equivalents) under a single surgeon (Senior author - RJM). Data
collected on all patients included: Oswestry Disability Index (ODI),
Short Form 12 (SF-12) v1, Visual Analogue Scale (VAS) and Patient
Satisfaction Index (PSI), length of hospital stay, time to mobilise,
postoperative medication and complications. Inclusion criteria
consisted of patients aged 18-75 with degenerative pathologies only
included. All patients complained of either back pain, radiculopathy,
claudication or a combination of these three symptoms. All patients
had pain resistant to prolonged (at least six months) conservative
therapy.
The ODI and SF12 were utilised to analyse the impact of these
surgical techniques on patient disability and quality of life, whilst the
VAS assessed pain. Both groups showed significant improvements in
quality of life and reduction in disability following their operations,
with ODI falling from 54% to 22% for the MIS technique (P<0.0001)
within the mean 16 month follow-up time period, and from 52% to
28% for the open technique (P<0.0001). Significant reductions in
pain postoperatively were observed following each technique, with
VAS falling from 7.9 to 2.4 for the MIS technique (P<0.0001) and
from 8.2 to 3.3 for the open technique (P<0.0001). Postoperative pain
was significantly lower following the MIS technique (2.4 vs. 3.3), but
despite this, the amount of pain relief (VAS change) provided by both
procedures were not significantly different.
A similar proportion of MIS (83.33%) and open (78.57%) patients
were satisfied undertaking surgery for the benefit they received with
their procedure. However surgery met the expectations of a significantly
greater proportion of MIS patients than open patients (P=0.0236).
The results for PSI are illustrated in Figure 6. The minimally invasive
technique resulted in significantly shorter hospital stay (P=0.0016) and
time to mobilise (P=0.0021) after surgery than the open technique.
The MIS group had a significantly lower postoperative opioid usage
(85.90 vs. 168.9mg of IV morphine) than the open group (P=0.0130).
However the non-opioid usage between the MIS and open groups (26.9
vs. 30.84g of oral paracetamol) was not significantly different.
The minimally invasive cohort was found to have significantly
lower postoperative pain, and to have met the expectations of a
significantly greater proportion of patients than conventional open
surgery. The minimally invasive approach also had significantly shorter
length of stay, time for mobilisation, lower opioid use and a reduced
total complication rate. In our study minimally invasive techniques
provide similar efficacy to the conventional open technique, and proves
to be superior in regards to patient satisfaction, length of hospital stay,
time to mobilise and complication rates.
Discussion
Posterior lumbar decompression and fusion is an evolving
technique in an attempt to provide symptomatic and functional
relief from a complex degenerative process. There are currently
multiple alternatives to approach the pathology of degenerative
spondylolisthesis which potentially creates a decision and management dilemma. The SPORT trial, spondylolisthesis arm, concluded that
operative management provides superior results when compared to
non-operative management [1].

Figure 6: Patient Satisfaction Index. 1 – Surgery met my expectation, 2 – I did
not improve as much as I had hoped but I would undergo the same operation
for the same results, 3 – Surgery helped but I would not undergo the same
operation for the same outcome, 4 – I am the same or worse as compared
to before surgery.
PLIF has been shown previously to provide high fusion rates that
are at least equivocal, if not superior than postero-lateral fusion, with
potential for correction of the spondylolisthesis and improvements
in coronal and sagittal balance [8]. However, there is significant
morbidity involved with regards to intra-operative blood loss, postoperative
wound pain and delayed mobilisation post-operatively with
the traditional ‘open’ approach. Minimally invasive pedicle screw
fixation and minimally invasive TLIF using the METRx (Medtronic,
Memphis, USA) system has been combined previously with the authors
advocating: decreased blood loss, wound pain and average length of
post-operative hospital stay. They do acknowledge, however, that the
limited exposure does provide a potential environment for an increased
chance of adverse events intra-operatively and a reduced operative field
to correct any adverse event such as an unintended durotomy. Previous
literature reveals that intra-operative durotomy rates are significantly
increased, and the length of the procedure is also increased [7,9,10]. By
providing an open laminectomy and PLIF procedure, the caveats of the
minimally invasive TLIF/PLIF are avoided but with retention of the
benefits of the percutaneous pedicle screws.
One potential source for increased post-operative wound pain
is muscle dissection off the facet joints and transverse process. For a
traditional open fusion, this is necessary to provide exposure for the
pedicle screw entry points, especially the most rostral screw. Using
percutaneous pedicle screws allows for minimal muscle dissection and
avoidance of this morbidity.
Another potential source for increased post-operative wound pain
is far lateral muscle dissection off the transverse processes to allow for
a posterolateral graft. As this operation involves PLIF alone, no lateral
dissection of muscle off the TP’s is necessary.
Finally, in combination with the above two pain prevention
strategies, the smaller exposure required both laterally and craniocaudally,
allows for a more minimalistic incision that provides less
soft tissue dissection, without compromising access. Wound size has
previously shown to be independent of post-operative pain [11], but
at the very least it is logical that a smaller wound facilitates reduced
muscular exposure, and greater patient satisfaction.
The senior author (RJM) has performed 53 “80/20” type procedures
for degenerative spondylolisthesis. To date, no patient has required a
blood transfusion with the average length of stay less than 3.7 days. In
addition, over 50% of patients have not required morphine/narcotic
based analgesia in the postoperative period.
Conclusion
The “80/20” approach proposed by the authors has been
successfully employed at our institution with encouraging results.
The method of open PLIF and percutaneous pedicle screw fixation
allows for minimisation of muscular dissection to reduce morbidity,
reduce postoperative pain medication requirements and allow
earlier mobilisation, whilst providing effective decompression and
stabilisation of the degenerative motion segment.
References
- Weinstein JN, Lurie JD, Tosteson TD, Hanscom B, Tosteson AN, et al.
(2007) Surgical versus nonsurgical treatment for lumbar degenerative
spondylolisthesis. N Engl J Med 356: 2257-2270.
- Yan DL, Pei FX, Li J, Soo CL (2008) Comparative study of PILF and TLIF
treatment in adult degenerative spondylolisthesis. Eur Spine J 17: 1311-1316.
- Cheng L, Nie L, Zhang L (2009) Posterior lumbar interbody fusion versus
posterolateral fusion in spondylolisthesis: a prospective controlled study in the
Han nationality. Int Orthop 33: 1043-1047.
- Kim KT, Lee SH, Lee YH, Bae SC, Suk KS (2006) Clinical outcomes of 3 fusion
methods through the posterior approach in the lumbar spine. Spine (Phila Pa
1976) 31: 1351-1357.
- Dehoux E, Fourati E, Madi K, Reddy B, Segal P (2004) Posterolateral versus
interbody fusion in isthmic spondylolisthesis: functional results in 52 cases with
a minimum follow-up of 6 years. Acta Orthop Belg 70: 578-582.
- La Rosa G, Conti A, Cacciola F, Cardali S, La Torre D, et al. (2003) Pedicle
screw fixation for isthmic spondylolisthesis: does posterior lumbar interbody
fusion improve outcome over posterolateral fusion? J Neurosurg 99: 143-150.
- Park Y, Ha JW (2007) Comparison of one-level posterior lumbar interbody
fusion performed with a minimally invasive approach or a traditional open
approach. Spine (Phila Pa 1976) 32: 537-543.
- Wang JC, Mummaneni PV, Haid RW (2005) Current treatment strategies for
the painful lumbar motion segment: posterolateral fusion versus interbody
fusion. Spine (Phila Pa 1976) 30: S33-S43.
- Foley KT, Holly LT, Schwender JD (2003) Minimally invasive lumbar fusion.
Spine (Phila Pa 1976) 28: S26-S35.
- Khoo LT, Palmer S, Laich DT, Fessler RG (2002) Minimally invasive
percutaneous posterior lumbar interbody fusion. Neurosurgery 51: S166-S181.
- Datta G, Gnanalingham KK, Peterson D, Mendoza N, O’Neill K, et al. (2004)
Back pain and disability after lumbar laminectomy: is there a relationship to
muscle retraction? Neurosurgery 54: 1413-1420.
Submit your next manuscript and get advantages of OMICS Group submissions
Unique features:
- User friendly/feasible website-translation of your paper to 50 world’s leading languages
- Audio Version of published paper
- Digital articles to share and explore
Special features:
- 200 Open Access Journals
- 15,000 editorial team
- 21 days rapid review process
- Quality and quick editorial, review and publication processing
- Indexing at PubMed (partial), Scopus, DOAJ, EBSCO, Index Copernicus and Google Scholar etc
- Sharing Option: Social Networking Enabled
- Authors, Reviewers and Editors rewarded with online Scientific Credits
- Better discount for your subsequent articles
Submit your manuscript at: http://www.omicsgroup.info/editorialtracking/spine/
 Minimally Invasive Spinal Fusion Ralph Minimally Invasive Spinal Fusion Ralph
You will need the Adobe Reader to view and print the above documents. 
|
